 |
| Nipah virus. |
How come one virus remains localised while the other goes systemic? And, more specifically how does it transport itself throughout the body?
Well, virus infection of a host is a complex multi-step process involving initial contact and entry into the organism (through the nose) , early replication in particular easy-to-access tissues (upper respiratory tract) and then in some cases the spread to specific tissue sites throughout the body (brain). It is these two stages of replication that most often or not lead to the development of disease yet just how does the virus traverse the gap between the two tissue sites - especially given the minute size of a virus particle?
There are probably three hypotheses of virus spread that could be correct here: lots and lots of virus particles could be released directly into circulation (lymph fluid and blood) from the early site of replication and our blood circulation could do the work for it; the virus could infect those immune cells that cluster around sites of virus infection - or are present naturally in the initial site; or finally, the virus could basically cling on to those highly motile immune cells and be trafficked around the body and effectively transfer infection to the blood vessels and other organs.
 |
| Could your white blood cells transport virus throughout your body? |
One group has recently asked this question with reference to nipah virus (read the paper here) and has discovered that this virus doesn't infect human immune cells although it does bind to them and this virus/cell interaction facilitates infection of other cells and may allow systemic spread.
They initially came at this problem at an in vitro level - albeit using cells taken directly from the blood of healthy volunteers. The group must have initially thought that nipah must directly infect white blood cells and this is how it spread - after all this is fairly common for other related viruses, such as measles. To determine exactly which cells supported virus replication they added a green fluorescent protein (GFP) - expressing virus to a panel of white blood cells derived from the blood of the healthy humans and specifically assayed for virus-mRNA synthesis, GFP expression and how much virus was released into the culture medium. Surprisingly only one cell type - dendritic cells (DC's) - an antigen-presenting cell - supported any kind of replication and even then it wasn't great (see below).
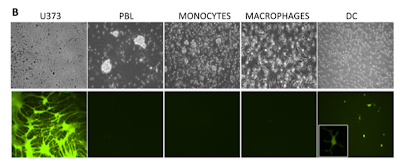 |
| GFP-nipah virus infects control neuronal U373 cells but not human immune cells - except DC's to an extent |
So how come nipah isn't so good at infecting these cells? Is it a receptor issue? Well the group looked at the mRNA levels of the two nipah virus receptors (Ephrin B2 and B3) in all the cells under investigation and found little correlation between their expression and the ability of nipah to infect them. For example, even the dendritic cell which had the lowest level of both receptors is able to support entry and replication while the other cells (macrophages and monocytes) that express higher levels of it fail to do so. The authors hypothesize that the DC's are engulfing nipah virus particles via a process known as macropinocytosis instead of via virus/receptor binding.
I mentioned earlier that the virus doesn't actually need to infect the cells to use them as an effective means of transportation - it can really get by through binding to the outer membrane of the cell much like a microbial hitch-hiker. So they looked at how much nipah virus was associated with each cell following stringent washes and surprisingly all the cells looked at were able to bind nipah virus particles even when they failed to get infected themselves.
But what exactly is blocking infection when the cells bind virus AND express receptor molecules on their surface - something is inhibiting entry. The paper doesn't really address this issue but points to a role of a virus receptor-independent molecule that binds to nipah virus particles yet prevents internalization and engulfment. And even more interestingly, these virus-laden cells were able to efficiently transfer the infectious particles to other cells - as shown with the DC's and PBL's below and this ability to 'trans-infect' was retained over a couple of days (see below).
 |
| Transfer of infection with virus bound to immune cells overlaid on top of other cells |
 |
| Hamster infections with nipah or nipah bound immune cells. |
So these cell-bound viruses are able to transmit infection in vivo, which points to it having a role in humans.
 |
| Current model for nipah infection and spread within the body |
Just one final thought: watch this video below first - imagine this cell going about its normal routine of moving along your blood vessels and squeezing through them but with it covered in infectious virus; every cell ut encounteers will more than likely be exposed to virus and potentially become infected. No wonder nipah is such a deadly pathogen.
 Mathieu, C., Pohl, C., Szecsi, J., Trajkovic-Bodennec, S., Devergnas, S., Raoul, H., Cosset, F., Gerlier, D., Wild, T., & Horvat, B. (2011). Nipah Virus Uses Leukocytes for Efficient Dissemination within a Host Journal of Virology, 85 (15), 7863-7871 DOI: 10.1128/JVI.00549-11
Mathieu, C., Pohl, C., Szecsi, J., Trajkovic-Bodennec, S., Devergnas, S., Raoul, H., Cosset, F., Gerlier, D., Wild, T., & Horvat, B. (2011). Nipah Virus Uses Leukocytes for Efficient Dissemination within a Host Journal of Virology, 85 (15), 7863-7871 DOI: 10.1128/JVI.00549-11

















Nice post, and the video is really great. I knew virus's could hijack their way into cells, I didn't realise the blood cells could carry them around the body that much!
ReplyDeleteJust to ask - would you be interested in submitting this (or any other of your posts) to the MolBio carnival? We're currently looking for submissions for the August edition. http://molbiocarnival.blogspot.com/
Thanks for the comment - yeah it was pretty amazing to see this, mostly people just look at infection of cells but they should really look at what's stuck on to them!
ReplyDeleteI have just submitted it there to your site :) - I did not know this existed!! Keep up the good work
Nice post Mr Connor,could you please explain why NiV attack people in Bangladesh? is it artificial bioterorism or experimental of new bioterorism agent? because the NiV reservoir (bats) widespead in the word? and drinking raw date palm sap have been maybe for along time before NiV outbreak occur, and in our country drinking raw date palm sap also have been a habit and here is the habitat of the fruit bats.
ReplyDelete