What if all those vaccines - those ones that work really well - all stopped working? Imagine if the viruses and bacteria from which they are trying to protect you against, evolved and adapted to life in a largely immune population? Those robust antibody and T cell responses generated within a person following vaccination supply the perfect breeding ground for the selection of resistant mutants where anibodies can no longer recognise and neutralize their targets and where T cells fail to eliminate infected cells. So, is it possible and is it happening?
Well, we already know this kind of phenomenon from influenza, right? Every year we have to change the strains that are put into your flu jab to match those viruses predicted to be circulating come winter. This is based on generating an antigenic match of vaccine to wild virus; specifically, their surface HA proteins must look the same. This is why there has been such a push to develop universal influenza vaccines capable of immunizing people against all flu strains. For viruses like measles and mumps however, we have our universal vaccine, or at least we thought we did.
One of the fears behind the recent examples of mumps outbreaks in populations across the world where there are even very
high levels of vaccination is that it may provide the very breeding ground for vaccine scape mutants. We have even been noticing this with other vaccines: pneumococci, hepatitis B, and hepatitis A.
It prompts us to ask the question: are current mumps viruses able to get
around vaccine-induced immunity, and if so, do we need to develop new vaccines?
I've talked about the hypothetical reasons that may explain the recent mumps outbreaks and one of these was that
current mumps viruses are adapting to life in a human population that is
immune to their infection, i.e it is evolving to escape our
vaccine-induced immunity. This is an extremely important question as - if true - jeopardizes half a century's efforts in mumps elimination and in itself poses a significant public health problem. And as demonstrated by this recent paper, countries are already searching for new and improved mumps vaccines to get around this issue - they are rapidly taking a leaf out of influenza's book. Yet perhaps it is too early to do this.
Secondary vaccine escape - where despite the vaccine generating sufficient immunity to a pathogen, the virus or bacteria fails to be neutralized during an infection either due to loss or waning of immunity or through changes in the viral antigenic proteins. However, this has been debated for viruses like mumps as it was always thought to be monotypic, that
is immunity to one mumps virus type will inevitably protect you against
every other mumps strain out there, basically: to your immune system, all mumps viruses look identical. This is why our mumps universal vaccine works so well.
This thinking has run contrary to what's
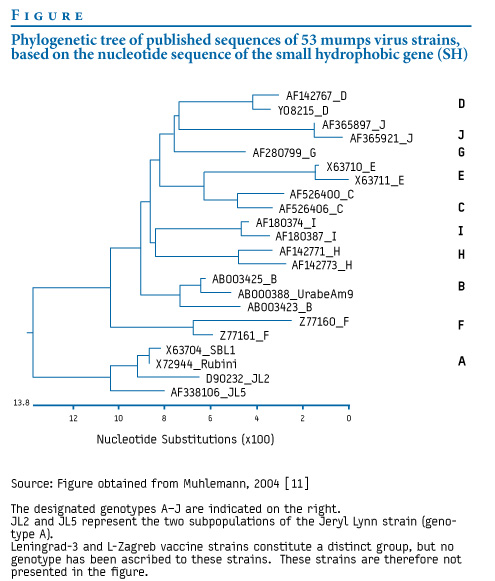
known about the great genetic diversity present in mumps - and really any RNA virus out there. When we explore the genetic sequences from all mumps viruses discovered, you can organize them in to a number of groups known as genotypes. These genotypes form clusters of closely related virus sequences of which there are around 12 or 13. Yet it has always been thought that immunologically speaking, this diversity didn't matter. This is especially relevant when you realize that our mumps virus groupings are based on an immunologically irrelevant viral gene. But consider that the most used vaccine strain, Jeryl-Lynn comes from genotype A, what are the odds that a virus from another genotype would look different and be able to get by the Jeryl-lynn induced immunity? This thinking gets worrying as no such outbreaks have occurred by viruses of the same genotype of the vaccine strain.
In order to get a better understanding of this, researchers from the Food & Drug Administration and Queen's University, Belfast (Disclaimer: this is the group I am a part of) decided to look into this in more detail. In a relatively simply designed study (published here, in the Journal of Virology), they took antibody serum from children recently vaccinated against mumps and used it to try and inhibit infection with a panel of viruses representing known mumps virus antigenic diversity.
Doing this they would be able to tease out whether genotype A-induced immunity was substantially able to protect against the virus in vitro. In doing so they also determined the major antibody targets of mumps vaccination using a range of recombinant viruses.What they found was that vaccine-induced immunity was able to effectively neutralize all groups of mumps viruses despite slight antigenic differences, i.e even though the viruses looked a bit different, they all looked sufficiently similar to the vaccine virus to be inhibited. So can we still say that secondary vaccine escape is occurring?
There are a few things to be aware of in this study: one, they focused on recently vaccinated children yet all outbreaks occurred in University-age Adults when they will significantly lower antibody responses due to waning immunity. Remember that secondary vaccine escape involves both loss of immunity and changes in viral proteins so how would the above results differ if lower antibody responses were considered? We'll have to wait for that, especially as this has already been suggested - along with antigenic differences - to play a major role in these outbreaks. The final point is that they only studies B cell response and not T cell ones, although it is thought that T cells play little role in protecting against mumps.
But what this work does add to is the already growing precedent that current mumps vaccine regimes - while generally working very well in the past- may not be sufficient to protect against and eradicate all strains of mumps in the future when waning immunity is taken into consideration. Luckily, we can get around drops in antibody levels through catch-up booster vaccines, so should we be looking out for MMR catch-ups in the coming future?

No comments:
Post a Comment
Markup Key:
- <b>bold</b> = bold
- <i>italic</i> = italic
- <a href="http://www.fieldofscience.com/">FoS</a> = FoS